Insulin sensitivity is a topic that people in the fitness industry are very interested in.This is easy to fix as long as the pathophysiological mechanisms that make it up are known, which will be briefly described in this article, likewise, a series of supplements that can help with the improvement of said marker will also be described.
So, based on this, a series of simple stacks will be discussed and provided, available to everyone, that can be used to improve insulin sensitivity depending on the phase in which we find ourselves.
Glucose intolerance
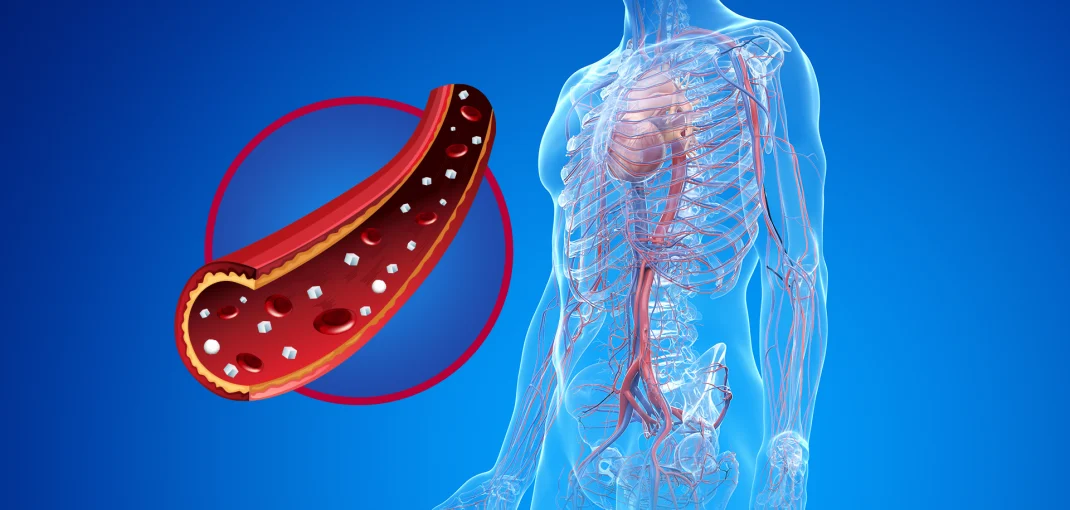
On average, a healthy adult human being has about 90mg/dL of glucose in an 8-hour fasting state; the normal level ranges from 70 to 110mg/dL, qualifying any measurement between 110 and 125mg/dL as pre-diabetes and from 126mg/dL onwards, as diabetes.
Insulin is secreted by the Pancreas in response to the alterations it perceives in blood glucose levels, so although glucose levels remain more or less within a few limits throughout the day, insulin levels fluctuate quite a bit. depending on the meals we make.
Insulin has a receptor on the cell membrane in tissues such as muscle where, once it binds to it, a cascade of molecular signaling is initiated (which has Akt phosphorylation as the last step) with the aim of inducing the migration of glucose transporters (GLUT) from the cytoplasm to the cell membrane to take up glucose.
And what happens when glucose levels are low? Well, for that, the pancreas, in addition to having beta cells that secrete insulin, also has alpha cells that secrete glucagon.
Glucagon is a hormone that exerts several functions but all with the same purpose: to stimulate the production and release of glucose and to inhibit glycolysis (burning of glucose).
Summarizing:
- It stimulates the amount of amino acids taken up by the liver to produce glucose (neoglucogenesis).
- It stimulates the release of catecholamines.
- Stimulates the release of liver glycogen in the form of glucose.
- Stimulation of the creation of ketone bodies.
The curious thing about Glucagon is that its release is not regulated based on blood glucose, but based on the release of insulin by the beta cells of the pancreas, so it can be said that its secretion is based on paracrine regulation. ; so if they “see” that the pancreas is secreting insulin, it can be said that they intuit that glucose levels are high and therefore do not release anything, if on the contrary, they see that the beta cells are hardly secreting insulin They sense that glucose is low and get to work.
Type 2 Diabete
With this more or less explained, we can move on to the next point and that is to explain what the hell type 2 diabetes is.
Type 2 diabetes, which is insulin resistant diabetes (which is because you are resistant to insulin), is characterized by a combination of:
insulin resistance
It is understood as such the phenomenon in which when insulin binds to its receptor on the surface of the cell membrane, the intensity with which the intracellular signaling cascades are produced is weaker, therefore, there is not as much displacement of insulin. GLUT receptors per unit of insulin, do you remember that the transport of fats to the mitochondria was inhibited and the amount of fatty acids present in the cell increased?
Well, this is what produces insulin resistance.
Therefore, taking into account the normal physiology of the human being, what is responsible for insulin resistance is nothing more and nothing less than a caloric surplus, since insulin resistance is nothing more than a cellular defense mechanism against excessive caloric consumption, since by preventing glucose from entering the cell, it increases fatty acid oxidation, reducing lipotoxicity due to lipid accumulation and thus, lipoapoptosis (cell death induced by excessive lipid accumulation ), in fact, according to tests carried out by Unger & Scherer in 2010, it is known that there is a positive correlation between adipose tissue (it must be well vascularized and with a high proliferation capacity to be considered metabolically healthy adipose tissue) and sensitivity to insulin, i.e.extremely obese subjects are extremely sensitive to insulin, although this is another topic to talk about.
Pancreatic cell dysfunction
If you have understood the above information, this will be very easy for you.
Do you remember the accumulation of fats inside the cell? Well, this produces what is called ectopic lipid deposition (in addition to the release of different undesirable adipokines), which is nothing more than the accumulation of fat outside the subcutaneous adipose tissue (visceral fat), this fat is extremely “unhealthy”. ”, so among other things, it produces the aforementioned lipotoxicity and with it, lipoapoptosis.
When it occurs in the pancreas, in the beta cells, this causes them to no longer function as they should and therefore, they do not respond as well to changes in blood glucose. More importantly, however, the same is true of the alpha cells of the pancreas; due to lipotoxicity, they become resistant to insulin, so they are constantly secreting glucagon (hyperglucagonemia), which is why diabetic subjects, even when fasting, have such high glucose levels, as well as using strips of ketone bodies in type 1 diabetes to assess the risk and severity of ketoacidosis.
Also, this is the reason why drugs like Metformin or Berberine work so well; because they inhibit hepatic neoglucogenesis.
Maintain and improve your insulin sensitivity
First of all, it should be noted that changes in lifestyle have much more significant effects than supplements: so do not forget that it is essential to first analyze and recognize what factors may be negatively affecting these and solve them as quickly as possible. (that’s a fancy way of saying shut the fuck up and stop eating, you swine), otherwise the best you can do with the use of supplements (and drugs) is to slow down the progression.
Now, before delving into the supplements, you must first understand the main underlying mechanisms of these:
AMPK
In the medical world, AMPK is often thought of as the antagonist of mTOR, that is, the hero that will end the pro-carcinogenic reign of the evil mTOR, so to speak. Others, such as most of the FItnes community, think of AMPK as the enemy to beat as it negatively affects muscle mass gains, and mTOR as the hero of the movie… and I think it goes without saying that neither of these two points of view is correct, right?
AMPK and mTOR aren’t even necessarily antagonistic, at least not for the average person, that is, people who train on a regular basis. For example, after a workout mTOR expression is at its peak, which occurs in the presence of increased AMPK expression.
What may at first seem like a paradox is actually easily explained if, instead of looking at the characteristic downstream effects of mTOR and AMPK, we pay more attention to the circumstances in which they are activated.
With the activation of mTOR by the abundance of nutrients, specifically protein, and even more specifically leucine, one would not expect to see increases in AMPK at the same time. After all, the latter is expressed when a cell detects a lack of nutrients in the form of an increase in ADP (indicative of ATP used) and a decrease in ATP levels. The reaction, that is, increased expression of AMPK, will have further effects on glucose uptake and fatty acid oxidation, both of which contribute to the restoration of normal ATP levels in the cell.
Both AMPK and mTOR act in a highly localized manner. Exercise-induced glucose uptake is therefore muscle-specific, which should be obvious, since exercise will raise ADP levels only in muscle. Supplemental agents that mimic this effect, on the other hand, act systemically.
Therefore, agents such as alpha-lipoic acid or Metformin (which will work systemically) will increase glucose uptake in both muscle and adipose tissue (Moini, 2002). After a workout and at other times, where glucose uptake is already high and, more importantly, muscle-specific, it’s not necessarily the best idea to try to “intensify” the effects by using one class of supplements which are often mislabeled as “insulin mimetics”.
PPAR-gamma
If you read about the effects that each of the different PPARs have, you can easily deduce that if you block PPAR-gamma, you can inhibit energy uptake by adipose tissue.
This, which at first seems to be the cane, is not at all as beneficial as you think. For example, it is quite likely that CLA-induced PPAR-gamma blockade (in rodents) is also responsible for the higher propensity to develop NAFLD in rodents.
The Fedor & Co. results show that these effects can be enhanced if the PPAR-gamma suppressor (ie, conjugated linoleic acid) is combined with a supplement that exerts the opposite effects on the liver; DHA from fish oil.
The latter, like many of the older diabetes drugs, is a PPAR-G agonist.
Whether PPAR-gamma blockade is good or bad obviously depends on the scenario we are talking about. For a low-fat individual who exercises regularly and wants to reduce as much as possible the accumulation of body fat in a hypercaloric diet environment, it is possibly a good thing, since hardly, thanks to physical exercise and controlling their body fat percentage, there is no accumulation of fat at the liver and visceral level in general.
However, in the case of obese and sedentary individuals, especially in the context of a hypercaloric diet, these would be completely contraindicated.
As paradoxical as it sounds, the antidiabetic effects of thiazolidinediones (TZDs), which are PPAR-gamma activators, which are still used to “treat” (or rather, “manage”) diabetes and other diseases that present in the form of insulin resistance, they exert their effects at the expense of increased body fat storage. The latter can become quite pronounced.
How can I know if I am insulin resistant?
Normally, it is often said that if after a meal high in carbohydrates you feel lethargic or if you see that a high consumption of these “covers you up”, you are resistant to insulin.
Personally, I would say that if these are the main signs you rely on to determine your glucose tolerance status, there is a good chance that you will be misdiagnosed.
To assess your glucose sensitivity status, one of the best and least invasive ways is simply to do a HOMA-IR (which is nothing more than a value that is taken based on your insulin level and fasting glucose), and if possible, combine it with a cortisol measurement to rule out the possibility of a false positive due to a dawn phenomenon due to the stress that taking the test may be generating (although even in the worst case, the HOMA-IR should be within normal parameters).